A Diabetic Product Review for Non-Diabetics - The Medtronic MiniMed Paradigm "Revel" Insulin Pump and CGM
 This is a review for Diabetics. If you're not a diabetic, consider this and it might help you enjoy this review. This is a product that will never affect your life. You've probably not thought about how an insulin pump works or its features. Here's a nice analogy I use to explain how diabetes works. It's called Diabetes: The Airplane Analogy.
This is a review for Diabetics. If you're not a diabetic, consider this and it might help you enjoy this review. This is a product that will never affect your life. You've probably not thought about how an insulin pump works or its features. Here's a nice analogy I use to explain how diabetes works. It's called Diabetes: The Airplane Analogy.
I've just received an upgrade to my insulin pump and I'm thrilled. Products like this are as important to us (diabetics) as your phone, your fancy remote control, your new DVD Player. I touch this device as often as my phone. It's attached to me 24 hours a day, it's an "external organ" to me. I've worn an insulin pump every day, all day (except showers) for the last decade.
If you find this interesting, please consider helping fight diabetes: http://hanselman.com/fightdiabetes or tweeting the link http://hnsl.mn/fightdiabetes
I've had Medtronic pumps since 2000. I upgraded to a Paradigm with a CGM "Continuous Glucose Meter" in 2006. Last week I upgraded to a new Paradigm "Revel" Insulin Pump with a number of new features. Insulin Pumps have come a long way since they were backpacks.
If you're not familiar, here's some diabetic equipment basics.
Diabetes Basics
 I'm a Type 1 Diabetic. That means my body produces no insulin of its own and I need to get insulin from outside sources. When I eat food, the sugar in my blood goes up and isn't delivered to my cells and my body starves while marinating it its own sugar. When I take insulin, my cells unlock, sugar (fuel) is delivered to the cells, and my blood sugar values go down. Eat, go up, take insulin, go down.
I'm a Type 1 Diabetic. That means my body produces no insulin of its own and I need to get insulin from outside sources. When I eat food, the sugar in my blood goes up and isn't delivered to my cells and my body starves while marinating it its own sugar. When I take insulin, my cells unlock, sugar (fuel) is delivered to the cells, and my blood sugar values go down. Eat, go up, take insulin, go down.
What's a Blood Sugar Meter do?
It does just that, it measures the level of sugar in my blood. I prick my finger, usually 10 times a day or so, and I put the drop of blood on a small gauze strip that goes into a machine and gives me a number. If it goes high too long, I'll die slowly. If it goes low too long, I'll die quickly. So, we need to keep that number as close to number as possible.
What's an Insulin Pump do?
 I took manual shots for 5 years. Some diabetics take just a few shots, 3 or 4, using a mix of short-acting (take a few hours) and long-acting (spreads over 12 or 24 hours) insulin. Others use a MDI (Multiple Daily Injections) technique, as I did, taking as many as 6-10 small shots of insulin a day. This is not uncommon and is often referred to as the 'poor man's pump.'
I took manual shots for 5 years. Some diabetics take just a few shots, 3 or 4, using a mix of short-acting (take a few hours) and long-acting (spreads over 12 or 24 hours) insulin. Others use a MDI (Multiple Daily Injections) technique, as I did, taking as many as 6-10 small shots of insulin a day. This is not uncommon and is often referred to as the 'poor man's pump.'
As a diabetic, once you've started taking that many shots, you get tired of taking shots. Enter the insulin pump. Once every 3 to 6 days, you poke a longish needle into your fat, then pull it out leaving a soft plastic canula embedded in you and held with tape. The insulin is sitting inside the pump and is pushed by a motor in the pump, slowly, through a long tubing and into you.
Now you can make tiny manual adjustments all day without shots. It's like the difference between making large, coarse movements of the steering wheel while driving and making those tiny back and forth adjustments you make just to say in your own lane on the road. Insulin pumps allow you 10-20x more precision over shots.
Everything inside an Insulin Pump is manual. It does nothing automatically other than a small background amount of insulin. My insulin pump gives me more control and means I get poked less often. But, it's not automatic. It doesn't cure or solve Diabetes.
So, to review. I did shots for 5 years, then a fairly standard insulin pump for 5 years. Then I got a CGM.
What's a CGM (Continuous Glucose Meter) do?
 Pricking your finger and check your blood sugar tells you your sugar level now, but not 5 minutes ago, nor does it show the trend. Hey, my sugar is 80! Was it 200 a half hour ago? Or was it 50 a half hour ago. A single sugar value is about as useful as a single speed value or a single altitude value.
Pricking your finger and check your blood sugar tells you your sugar level now, but not 5 minutes ago, nor does it show the trend. Hey, my sugar is 80! Was it 200 a half hour ago? Or was it 50 a half hour ago. A single sugar value is about as useful as a single speed value or a single altitude value.
A CGM, or Continues Glucose Meter, is a transmitter that sits inside you body, usually inserted with a needle and a sensor then uses tiny micro-currents against your body's interstitial fluids to estimate (extrapolate) your blood sugar. It doesn't test blood and they are not typically very accurate. In fact, they have a little disclaimer that effectively says "don't make decisions using these values."
CGMs do not replace finger sticks. They are not as accurate, but they provide valuable slope data that diabetics need. Accurate single value readings via finger sticks, combined with not-as-accurate slope information, combined with the ability to easily give myself small or large amounts of insulin without shots (I change the pump every 3 to 6 days, that does involve a needle) means I've got the information I need to maintain good control.
The Paradigm series of pumps are an Insulin Pump, but also a CGM receiver. They talk wirelessly to the CGM transmitter (see the picture above that is not my stomach) as well as wirelessly to a finger stick blood sugar meter. It's all one integrated thing.
Now, what's new in this new pump?
Medtronic MiniMed Paradigm "Revel" Insulin Pump
To review, insulin pumps are not automatic. They don't deliver without me saying so. While the pump talks wirelessly to meters and CGMs and stores values in memory, it doesn't act on them. There is no "closed loop" system. The delays involved are too great. However, the new "Revel" pump does add a number of cool new features that are making my life easier already. I think it's a great upgrade and if you have a MiniMed pump you should try to upgrade with their "Pathway Program." It's worth it.
New Features
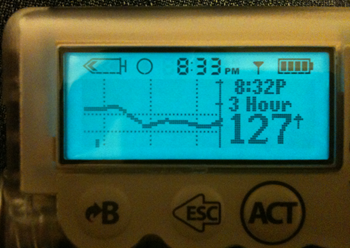
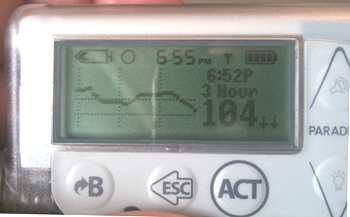
Better charts. Previously the charts were either 3 hours or 24 hours. Far to zoomed in, or so far out as to be useless. Now you can zoom 3, 6, 12, 24. Here's some screenshots:
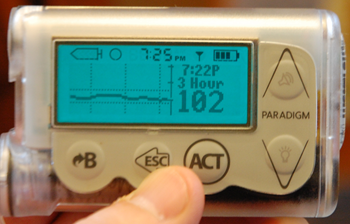



It was amazing how this apparently small upgrade changes the experience with the pump. The 6 hour view is a dream.
Predictive Alerts
This is the killer feature that has already helped me at least twice a day in the last week. The new Revel has a "rate of change" detection algorithm that is totally user-settable. If the pump decides that you will hit a high blood sugar if your current rate of change goes unchecked, it'll let you know via an alarm. This is the one feature I always needed and it works just as you'd wish it did.
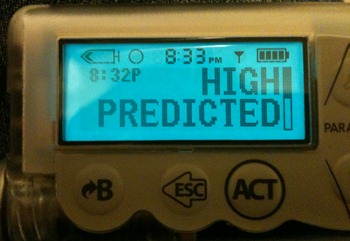
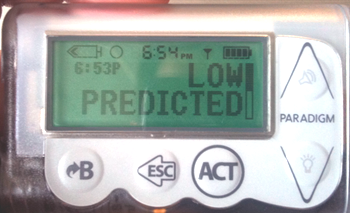
This feature did initially cause me to stack insulin a bit and caused a few lows as I was acting extra aggressively to squash highs, but I am finding I'm getting used to it. I wish it hadn't taken 5 years to get it. That's the tragedy of medical devices. You're thrilled with your multi-touch color screen portable device and I'm happy if I get one firmware update every 5 years. The difference is, my phone crashed twice today. This pump has never crashed in 10 years. We sacrifice innovation for stability.
Subtle but Important Improvements
One of the most important numbers for a pumper is the amount of insulin that's "pending" or "active." Most insulin takes about 3-4 hours to get out of my system, so if I take 5 units now, and 5 more units in an hour, that's stacking doses. If I remembered or was told that I had ~5 units active, I might not have taken that second dose and could avoid a nasty low. The Revel automatically calculates the active insulin and shows you it in three new places. First, on the status screen, second in the manual bolus (dose) screen, and again on the Bolus Wizard. It was buried in the UI before, now it's front and center.
The motor is more precise now, letting you do basal rates as low as 0.025 units per hour, crucial for young people.
Conclusion
This upgrade, the Revel, makes a great pump better. It was totally worth the $399 Pathway upgrade. If you're on a Minimed pump, get the upgrade. If you're not on a pump, consider getting one, it'll change your life.
If you found this interesting, please consider helping fight diabetes: http://hanselman.com/fightdiabetes or tweeting the link http://hnsl.mn/fightdiabetes
About Scott
Scott Hanselman is a former professor, former Chief Architect in finance, now speaker, consultant, father, diabetic, and Microsoft employee. He is a failed stand-up comic, a cornrower, and a book author.
About Newsletter
I like your comment about stability over features. The stability and reliability of these things is phenomenal. It actually scares me a little bit when I think about the fact that they run on software.
Good anecdote, I finally got through all of the insurance red-tape about a year ago to get the pump with CGMS support (mine was out of warranty, so I couldn't take advantage of the Pathway program). One night I get a strange error on my pump, and it resets itself. From the looks of it I lost all of my settings, which is annoying cause I've got to reprogram things, but I do it and go to bed. Wake up the next morning, all is well, but while I'm at work I decide I should probably call about this error in case the insurance company pulls the thing where they don't want to ok the upgrade to the new pump because my old one is still working. Talking to the tech support person, I find out that the error I got was considered a "critical error", and basically meant the pump was toast. Here's the thing, though, even though it was toast, it was still doing what it was supposed to, and doing it perfectly as far as I could tell.
They sent me a replacement in less than 24 hours (even though I was out of warranty), and all was good until my new pump arrived about a month later. But I'm still amazed that a piece of hardware and software could experience a critical failure, and still function well enough to continue to keep me alive. Amazing stuff.
"The difference is, my phone crashed twice today. This pump has never crashed in 10 years. We sacrifice innovation for stability."
I have worked in health care software for a while now and that concept is so hard for everyone to get their head around. It is so easy for basically everyone to point to typical software and ask why medical software is: Slow to create, old looking, dull, hard to test...
The thing that gets lost is failure is not an option. Data loss is not allowed. Giving someone the wrong answer is not permissible.
Thanks for the post!
Here in the States, you can point to the Food and Drug Administration (FDA) for why those descriptors are almost always true. The approval process takes some time (read several months of QA) to get it right and to weed out critical errors as Casey described. I had worked with medical instruments for some time (large blood analyzers and other assorted laboratory equipment - the big brothers to the finger prick sugar meters) and the systems were generally built on top of fault tolerant operating systems with microkernel-like architectures. Therefore a critical error such as Casey described could cause a failure in one portion of the software, but the core functionality could continue.
I came across some information regarding a closed-loop insulin pump or more accurately an artificial pancreas. Some context: I've been doing some work with JDRF (Juvenile Diabetes Research Foundation) for the past several months in an ongoing engagement. Right now I'm migrating parts of their Artificial Pancreas Project website into an ASP.NET web content management system as a proof of concept along the path to converting the entire site as well as possibly some additional web properties. As I've been migrating their content for this demo I've had a chance to read tons of diabetes related information. I'm not a diabetic myself and don't have any close friends or family who are so I didn't know much about the disorder (other than your previous posts, of course. The airplane metaphor makes it so clear.) After all the the content I've read I'm amazed at the innovations and research that this organization does for diabetics everywhere. Scott, you've been someone I've really looked up to as developer and technology evangelist I would like to emulate when I "arrive" at the expert developer level I keep striving for. I respect you even more considering the additional challenges you've overcome with diabetes. Tom Brobson (from the Artificial Pancreas website) writes a couple of fascinating blog posts about his experiences participating in the clinical trials of a prototype artificial pancreas if anyone wants to learn more.
I too am waiting for mine to get approved and get to me. I'm SO excited to be pumping again. :)
PS my last one was an omnipod and I was at a HUGE failure rating for my pods. Their ideas are GREAT and I think it's a great idea. Their technology seriously lacks. I'd never ever suggest someone go on the Omnipod. Minimed has the technology and experience to make work.
How would you say this pump affects your ability to do sports? I am taking shots myself (type 1 as well) - and I have always resisted going to a pump because I like being able to move - I am a former gymnast (injuries suck) so I still have the want to feel like I don't have to worry about some device being attached to me. Do you think a pump does any serious hindering of this?
The capabilities of this thing does sound very useful!
http://www.bayercontourusb.ca/
As a Type 1 Diabetic, who also just happens to be a software developer, I wanted to say thank you for your review of this new pump technology. I put in my order for the Medtonic MiniMed Paradigm "Revel" Insulin Pump and CGM the day before you added this blog post. I am really looking forward to seeing what the CGM can tell me about my blood sugar during the day as there are definitely quirks to my readings that I wish I understood better. I hope that the CGM will help me fine tune things even more as my A1C readings have been pretty good (6.3 last month) since I got my first insulin pump almost 5 years ago, but things can always be improved. I look forward to hearing more from you regarding your experience with this new pump and CGM as well as all of your insight on the developer side of things.
Thanks again,
Bill
@Melissa - I have been considering the Omnipod over the minimed and the ping. the whole idea of no tubes sounds really attractive to me. I hope, if thats the one I end up choosing, that i dont have your difficulties.
So many options to consider, hard to be sure I am making the right choice.
-chris
So instead they tried concentrated Humulin-R (1u = 5u of normal Humulin-R) but the Humulin-R doesn't seem to work very well. (Or at all; I had been taken off the normal Humulin-R about fifteen years ago because it seemed to have very little impact on my blood glucose levels.) My blood sugars range from 300 to 700 with it and I can't seem to find a working paradigm with it, even with the alternate dosing.
If I could get a 600ml or 1000ml reservoir the pump would be incredible -- I'm almost willing to change the reservoir every day. But after 25 years of diabetes my insulin resistance and extra body weight are simply too great.
Do you, or any other reader of your blog, have any advice as to what I might pursue to help solve this problem? My doctors want to keep trying various things but I simply can't miss any more work, and even if I could, the high blood sugars make me extremely irritable and tired.
I'm thinking that, if nothing else, I could look into the possibility of donating the pump -- but I believe that since it's a medical device the government will stomp all over that.
(Yes, my endocrinologist has been kind enough to inform me that at his recent conference my insulin consumption exceeded every other patients. Easily.)
As for reservoirs, mine is a 180U one, but there is a 300U one for the Paradigm pump. The 722, I think. Are you sure there's not an "Extended" reservoir?
I am a type 1, currently on the Omnipod. I resisted pumps for years, afraid of the idea of being tethered. I was so excited when the Omnipod came out and offered an alternative to the traditional, wired pump. Having been on the pod for a couple of years, I am very accustomed to the paramaters of pumping in general. I have been waiting and hoping for the integrated CGM, and recently heard that Minimed incorporated the technology along with predicitve capabilities in the Revel.
In searching for more info, I came across your blog. First off, thank you so much for sharing your experiences. I presume you do it for a reason, and I just wanted to let you know that it really helped this diabetic. Second, if you don't mind, I have a couple of questions. Do you notice having a second insertion site (the monitor)? I imagine that it is much like the pod-- since there are no wires, I forget it's there and it doesn't bother me at all. Given the fact that the CGM is not as reliable as fingerpricks, do you think the trade off of wireless pump to the wired version would be worth it? I realize this is a loaded question, and it's not meant as a challenge, rather, solicitation of input. Amazingly enough, I do no know any other T1's, despite living in a large city. I have to resort to feedback from strangers like you instead! Thanks again for the info you have already shared, and I appreciate anything further you can tell me.
I don't notice the CGM point and haven't had any problems with infection. That said, 3 or 4 times I *have* injected and for whatever reason, hit sensitive spots or "had a bad injection" where I felt like I was getting stabbed as I moved around. In those cases I just moved the needle.
Why not join a Type 1 Support Group?
Thanks for sharing what goes on with you being type 1. In previous years my exposure has been that a co-worker's son was type 1. So I helped raise money, rode my bike in fundraising efferts, etc. Now I've made a good friend who is also type 1, and I see how it affects her every day. Last night we put off dinner for an hour because 8pm was the "right time" to eat. She's got a Medtonic pump, but not any CGM gear, so I pointed her at this blog, and other imformation on CGM. As my friend said "I want to punch diabetes in the face, we can't have dinner until 8".
A great review. I'm a 68 year old, 722 pumper since 2006. Medicare forced a C-Peptide test to justify my 12/day BG test strip Rx reimbursement. Now my endo classified me as type 1 rather than the various new terms for adults, whose insulin making cell have died. I was having great difficulty maintaining BG control.
I bought a CGM to try to get a lower A1c (better BG control). It helped, but could not predict or notify me when my BG would rise unpredictably during sleep (dawn phenomenon or the Somogyi effect ).
I'm a retired control system engineer, who knew the value of predictive alarms. I learned of the Medtronic Pathway Pump Upgrade program and I am tweaking my refurbished 723 Revel pump now.
My BG still rises w/o me eating anything day and night. The 723's new CGM alarm features are helping me to lower my avg BG.
Again Scott that was an accurate review, that diabetics having BG control problems should be aware of.
Leslie
Comments are closed.
